Recent advances in nanotechnology are introducing materials that autonomously repair damage and actively combat bacterial colonisation, potentially transforming long-term restoration outcomes.
What You'll Learn in this article:
- The science behind materials that repair themselves - and why 4-hour crack healing could revolutionize restoration longevity
- How fillings now actively hunt bacteria - reducing secondary caries through sustained antimicrobial action at restoration margins
- Why these aren't just better composites - but therapeutic systems that continuously rebuild tooth structure
- The practice integration reality - no protocol changes needed, but significant competitive advantages available
- Timeline for adoption - what's available now, what's coming in 2-3 years, and how to position your practice
Recent advances in nanotechnology are introducing materials that autonomously repair damage and actively combat bacterial colonisation, potentially transforming long-term restoration outcomes.
Secondary caries remains the primary cause of restoration failure in clinical practice, driving the expensive cycle of replacement procedures that affects both patient outcomes and practice efficiency. Despite significant advances in adhesive systems and composite formulations, the fundamental challenge persists: traditional materials are passive components that cannot respond to the dynamic oral environment.
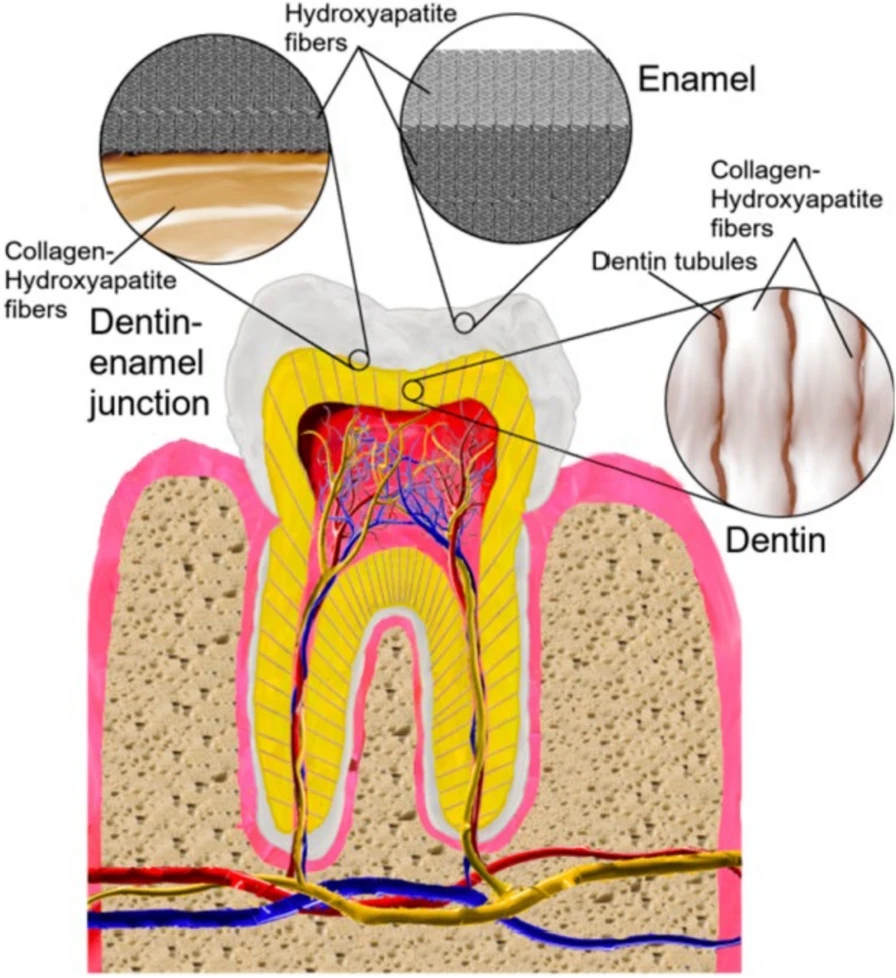
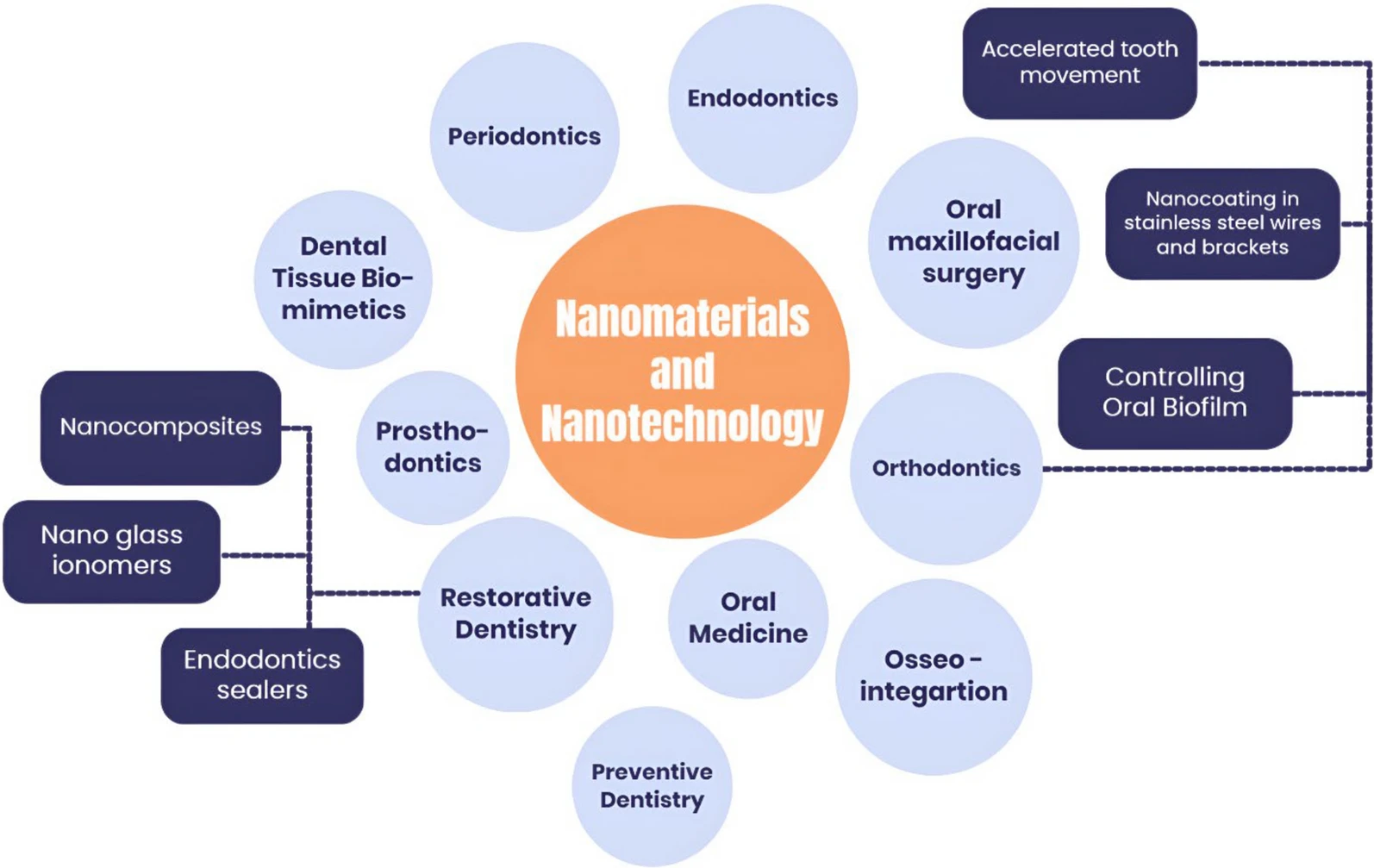
This limitation has prompted researchers to explore nanotechnology applications that transform dental materials from inert space-fillers into active therapeutic systems. The emerging evidence suggests we may be approaching a significant shift in how restorative materials function within the oral cavity.
Self-healing composite systems
The development of self-repairing dental materials draws inspiration from biological healing mechanisms. Research from Aalto University and the University of Bayreuth has demonstrated composite systems capable of achieving 80-90% structural recovery within four hours of microcrack formation, with complete integrity restoration within 24 hours.
The mechanism involves polyurea-formaldehyde microcapsules distributed throughout the composite matrix, containing reactive healing agents. When mechanical stress creates microscopic fractures, these capsules rupture and release compounds that polymerise autonomously, effectively sealing the damage before it can progress to clinical failure.
From a practical standpoint, this technology addresses one of the most frustrating aspects of restorative dentistry: the unpredictable nature of composite longevity. Current failure rates of 15-20% within seven years could potentially be reduced significantly, with projected lifespans extending to 15 years or more for appropriately placed restorations.
Antimicrobial nanotechnology integration
While mechanical self-repair addresses one aspect of restoration failure, the more significant development lies in materials that actively combat the biological causes of secondary caries. Studies led by Yue et al. at the University of Maryland have demonstrated composite systems that simultaneously heal mechanical damage, eliminate pathogenic bacteria, and promote remineralisation.
These materials incorporate precisely engineered silver nanoparticles that maintain sustained antimicrobial activity without compromising aesthetic or mechanical properties. The research demonstrates a four-log reduction in Streptococcus mutans colony formation while remaining below established cytotoxic thresholds. Quaternary ammonium compounds work synergistically to disrupt biofilm formation at restoration margins.
The third component involves calcium phosphate nanoparticles that continuously release beneficial ions, maintaining conditions favourable for remineralisation while buffering bacterial acid production. Tel Aviv University research confirms these nano-assembly systems demonstrate sustained bacterial inhibition with 67% reduction in biofilm formation compared to conventional materials.
Clinical implementation considerations
The transition from research to clinical application is progressing rapidly. Current nano-enhanced composites with improved mechanical properties have received regulatory approval and are being integrated into practices. These materials demonstrate 20-30% improvements in wear resistance and marginal integrity while maintaining compatibility with existing clinical protocols.
Placement techniques require no modification, bonding systems remain unchanged, and curing procedures follow established parameters. This compatibility removes the technical barriers that often impede new material adoption, allowing practitioners to benefit from enhanced performance without workflow disruption.
Cost analysis reveals initial material expenses run 15-25% higher than conventional composites. However, the economic equation shifts when considering reduced replacement procedures and improved patient satisfaction. Practices report enhanced case acceptance when patients understand the longevity benefits, creating opportunities for appropriate fee positioning.
Impact on restorative practice
These technological developments signal a fundamental evolution from repair-focused to prevention-focused restorative care. Traditional materials simply replace lost tooth structure, while bioactive systems actively maintain the oral environment to prevent future pathology. This aligns with contemporary emphasis on minimally invasive techniques and long-term oral health maintenance.
For practice positioning, early familiarity with nanotechnology-enhanced materials offers distinct advantages. Patients increasingly seek evidence-based treatments with demonstrated superior outcomes. The ability to offer materials with documented longevity benefits creates meaningful differentiation while strengthening referral relationships through demonstrated commitment to clinical innovation.
The educational component becomes increasingly important as these materials approach standard-of-care status. Practices that invest early in understanding nanotechnology applications will be better positioned for the inevitable transition.
Future developments
Current bioactive composites represent initial developments in what researchers term "intelligent materials." Advanced systems under development will respond dynamically to oral environmental changes, releasing therapeutic agents when pH drops or bacterial loads increase, essentially transforming restorations into active monitoring and treatment systems.
Self-healing formulations are entering Phase II clinical trials, with commercial availability projected within 2-3 years. Full antimicrobial systems are following closely, supported by accelerated regulatory review processes and robust safety data from extensive biocompatibility testing.
The evidence indicates that nanotechnology integration in restorative dentistry is transitioning from research curiosity to clinical reality. The materials demonstrate measurable improvements in longevity and bacterial resistance while maintaining familiar handling characteristics. For practitioners, the relevant question is not whether these technologies will influence restorative treatment, but how quickly they will become integrated into routine clinical practice.
The shift toward materials that actively participate in maintaining oral health represents more than incremental improvement. It suggests a future where restoration failure becomes increasingly uncommon and long-term maintenance of restorative treatment becomes the expected standard rather than the hopeful exception.




